The Principles of Wound Management
“Nurses are the heart of healthcare.”
– Donna Wilk Cardillo
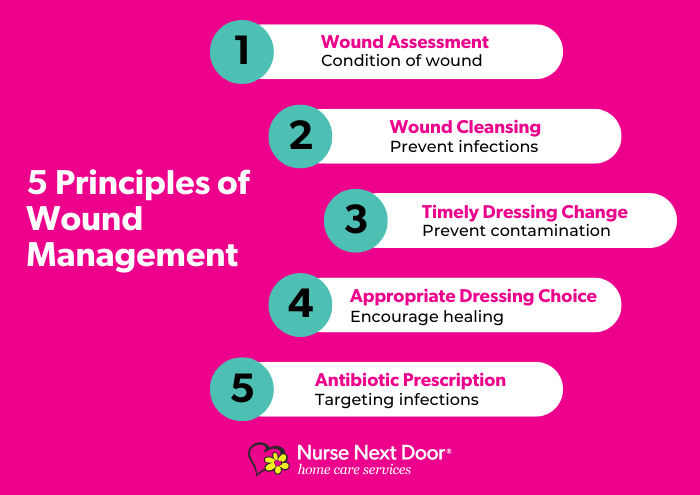
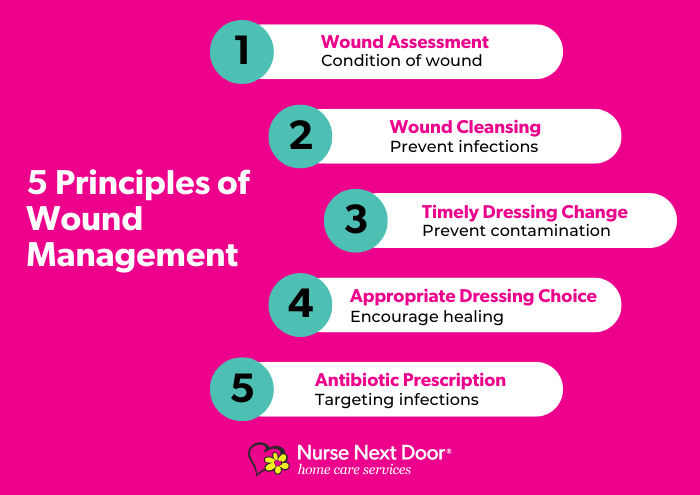
Wound management and wound care is a common practice for nurses in both hospitals and home care. The 5 principles of wound management provide health professionals in both hospitals and home care nursing with a guide to ensure their clients receive the appropriate treatments so they can continue to live as comfortably as possible.
1. Wound Assessment
2. Wound Cleansing
3. Timely Dressing Change
4. Appropriate Dressing Choice
5. Antibiotic Prescription
5 Principles of Wound Management
To achieve timely wound healing or prevent wound infection, healthcare professionals and nurses will follow general wound management practices so the client can remain as comfortable as possible during their recovery.
1. Wound Assessment
In the initial wound assessment, nurses will consider every aspect of an individual’s health and well-being as it may impact the healing process. Nurses will also look at addressing any vascular disorders, poor diabetic control, steroid use, inadequate nutrition and even smoking as all these things can delay a wound from being healed. If any ulcers are present, these areas will be a key focus as they do require pressure relief. Depending on the condition of the wound including aspects like tissue health, inflammation and moisture nurses will perform several actions during the wound cleansing process.
2. Wound Cleansing
Cleansing the wound surface will assist with successful wound healing and wound infection prevention as it will reduce the bacterial load and contamination. Sometimes, if sensible and practical, nurses will cleanse wounds by irrigation with each dressing change however this may depend on the nature of the wound and its healing process. In general, Irrigation with a syringe or a bag of sterile saline is poured slowly over the wound as part of the process.
3. Timely Dressing Change
Frequent review of the wound, as well as dressing changes, should be undertaken for any wound. Timely dressing changes are done when a dressing first starts to show tears or is contaminated. When changing dressings, nurses will avoid causing the client pain and skin irritation, by giving the client medication, using dressing adhesive remover and soaking dressings before removal. For complex and chronic wounds photographs may be taken to track the wound’s progress.
4. Appropriate Dressing Choice
Dressing choices can be challenging when dealing with complex or chronic wounds and will vary based on the condition of the wound. For example, a moist wound environment can determine the type of wound dressings required and whether negative pressure is necessary during application. As a general rule, an ideal dressing will be the simplest and most appropriate dressing available to meet the client’s needs. Dressings should both physically and microbiologically protect a wound, is non-toxic, non-allergenic maintain appropriate wound humidity. To encourage compliance from the client, and ensure dressings do not impact activities of daily living.
5. Antibiotic Prescription
While it is uncommon, where appropriate topical or oral medications may be prescribed by a General Practitioner to help manage any wound infections that were examined with a swap. If antibiotics are prescribed, should be used for the shortest possible period and targeted the likely bacteria causing the infection. For chronic wounds, where clusters of bacteria are suspected to be present, nurses will cleanse the wound with an antimicrobial irrigation solution.
Both acute and chronic wounds, whether complex or superficial, can use the principles of wound management as a guideline to ensure a wound successfully heals or is managed enough that the client can continue to lead a comfortable life. Wound care is within the skill set of all health professionals, no matter their background, as an essential aspect of medical practice in both hospitals and home care.


Types of Wounds
Wounds can either be acute or chronic and their healing process may vary depending on the wound itself.
Acute Wounds
An acute wound is a sudden injury to the skin. It heals at an expected rate of the normal wound healing process. These wounds can occur on any part of the body and vary from superficial scratches to deep wounds that can damage blood vessels, nerves or muscles.
Surgical Wounds
These are incisions purposely made by health professionals and cut with great precision. Surgical wounds are usually closed with stitches, staples or adhesive.
Traumatic Wounds
Traumatic wounds occur unexpectedly and can vary from a superficial skinned knee to deeper lacerations caused by sharp objects or abrasions caused by scraping of the skin against a hard surface.
Burns
A burn can be caused by heat or a result of radiation, radioactivity, electricity, friction or contact with chemicals. Burns can be superficial affecting only the first layer of skin, but can also affect deeper tissues and cause nerve damage.
Chronic Wounds
A chronic wound does not heal in an orderly set of stages like most other wounds would. These wounds are very slow to heal and at times may stop in a part of the healing process for example they could remain in the inflammatory stage for too long causing pain or discomfort to an individual. Chronic wounds can include, but are not limited, to:
- Diabetic foot ulcers
- Venous leg ulcers
- Pressure ulcers
Over 420,000 Australians are suffering from chronic wounds. Although it can happen to anyone, age and some chronic diseases will increase the risk of chronic wounds. Chronic wounds may take years to heal and in some cases, they will never heal and can cause a person to experience severe emotional and physical stress and pain. Proper wound care is a critical part of recovery and wound management is essential for people living with chronic wounds to minimise the spread of infection.
At Nurse Next Door, we are celebrating ageing and are passionate about Making Lives Better.
To learn more about The Power of Happier Ageing you can download our report
or contact us today on 1300 600 247 to discuss how Nurse Next Door can help you keep doing what you love.
